
Practice Perfect 798
A Missed Opportunity When
Prescribing Antibiotics
A Missed Opportunity When
Prescribing Antibiotics

In Practice Perfect 793, Diagnosing MRSA From a Sensitivity Report, we discussed how to diagnose methicillin resistant Staphylococcus aureus (MRSA) infections from a culture and sensitivity report. This is easy to do once you know what to look for (resistance to oxacillin or cefoxitin). But there is more information one can glean from a culture and sensitivity (C&S) report. In fact, this report can help us choose the best antibiotic to prescribe…that is, they would be, if the reports contained the proper information.
Now, you’re thinking, “Of course, we can use the C&S report to choose targeted antimicrobial therapy. That’s the whole point of the report.” I’m going to argue that without additional information that is NOT reported on a typical C&S report, it really boils down to guesswork. In fact, we are missing an opportunity to improve our antibiotic stewardship through a more logical choice of antibiotics. Additionally, the C&S report is typically used erroneously, and this is to the detriment of our patients.
The C&S report is typically used erroneously and this is to the detriment of our patients.
Let’s take a second look at the C&S report that I showed in Practice Perfect 793. Focus specifically on the “Organism 2” column, and think for a moment to answer this question: “What antibiotic would you give this hospitalized patient?”
As I mentioned, the first step is to notice that this organism is resistant to oxacillin and cefoxitin, so we most likely have MRSA (that was, in fact, the organism infecting the patient’s foot in the image). The next step is to choose the best antibiotic. This is where we actually get into trouble.
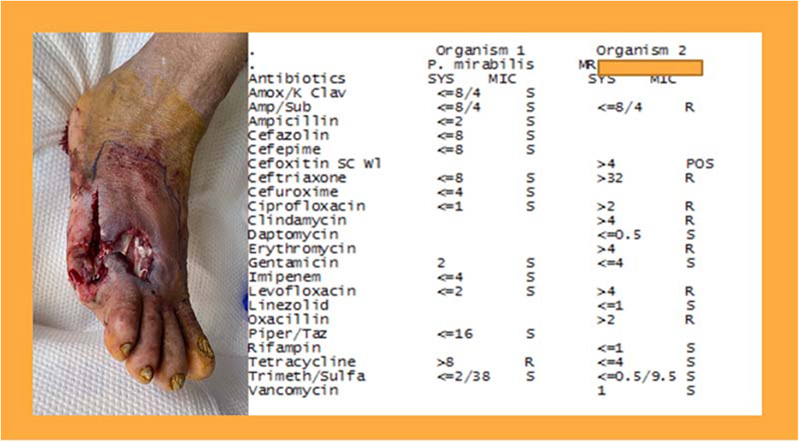
The typical approach is to find a drug that is reported to be “S” or sensitive for both organisms. Since this patient is in the hospital, we would choose an intravenous formulation. We should also consider cost, bioavailability, penetration into the tissues that are infected, and patient factors such as allergies or potential drug interactions. This would leave us daptomycin, gentamicin, trimethoprim/sulfamethoxazole, and vancomycin (I’m deliberately leaving out the drugs that are not reported for these microorganisms to make the discussion a little easier). How does one decide which one to use? For example, daptomycin is more expensive than vancomycin but is only once per day dosing versus vancomycin’s two times/day, but vancomycin has a greater renal toxicity risk. These and others are important considerations, but let’s boil this down to the question “which antibiotic is most likely to successfully eradicate this infection?
The key question is, “which antibiotic is most likely to successfully eradicate this infection?”
And here, my intrepid infection-treating friends, is where a major pitfall comes up. One might answer this question by looking at the minimum inhibitory concentrations (MIC) listed on the report and pick the one with the lowest MIC. That’s why it’s there, right? Wrong! An important concept to remember is you cannot compare MICs across different drugs. Each drug has different pharmacokinetics (drug absorption, metabolism, and excretion) so one MIC number does not compare with another. Why would a hospital report the MIC then?
Antibiotic Breakpoint
It would be useful if our hospitals reported another parameter, antibiotic susceptibility breakpoint, which we’ll call antibiotic breakpoint. To be completely honest, this is not a term I was taught in medical school, which is a shame. I only learned about antibiotic breakpoint while researching this topic. Antibiotic breakpoint is the concentration of drug at which bacteria become resistant. Since sensitivity is determined using dilution methods (commonly broth or disk microdiffusion methods) we can describe this as the dilution in which the organism becomes resistant. There is an antibiotic breakpoint reported for most bacteria and medications and is available from the Clinical and Laboratory Standards Institute (CLSI) in America. There’s also a European version called EUCAST. This is the number that is used to determine if a particular bacterial species is sensitive, intermediate, or resistant to a particular drug. The EUCAST report is easy to find, but the CLSI requires a login to their difficult to use website.
Determining Resistance Using the Antibiotic Breakpoint
When your hospital microbiology lab tests a culture you’ve taken, they determine an MIC for common antibiotics and then compare that MIC result to the reported CLSI value. They report the result of this comparison as the sensitivity. However, if our C&S reports listed the breakpoints, we would be able to use the information to compare the effectiveness of different drugs, which would allow us to choose the drug with the greatest potential benefit – a much more logical approach than the guesswork we currently use. Let’s look at a hypothetical example (Figure 1).
Figure 1. Pretend hypothetical antimicrobial sensitivity report for an imaginary Staph culture (reported in mcg/mL).
| Drug | Sensitive (MIC) | Intermediate | Resistant (breakpoint) |
| Fakecillin | 2 | 16 | 32 |
| Notrealosporin | 2 | 4 | 8 |
| Phoneymycin | 1 | 2 | 4 |
Comparing the number of dilutions needed for each drug to go from the sensitive MIC to the breakpoint would allow us to choose which drug to use. The rule here is the larger the number of dilutions means the organism is increasingly sensitive to the drug. To pick the best antibiotic, then, simply requires us to find out which drug has the greatest dilutions.
In our example, fakecillin takes 4 dilutions to go from 2 mcg/mL to 32. For notrealosporin it takes 2 dilutions, and for phoneymycin it also takes 2 dilutions. Because it takes more dilutions for the staph organism to become resistant to fakecillin, you would choose fakecillin (all other factors being equal).
What about our C&S report from above? Can we figure out a best antibiotic for this patient with a MRSA and Proteus infection? Figure 2 shows a comparison of the four drugs that we determined to be sensitive. To make things a little easier, I only used the data for Staphylococcus aureus. I’ll mention it was very difficult to find the data, and between the challenges of finding the data and my poor math skills, there’s a high chance the information is not accurate (caveat emptor!).
Figure 2. Sensitivity results compared with reported standard sensitivities showing reported breakpoints and calculated dilutions to resistance based on the MIC breakpoints (all measured in mcg/mL).
| Drug | Measured | Sensitive | Intermediate | MIC Breakpoints | Dilutions to resistance |
| Daptomycin | ≤ 0.5 | ≤ 1 | ---- | ---- | Many |
| Gentamicin | ≤ 4 | ≤ 4 | 8 | ≥ 16 | 2 |
| Trimethoprim/ Sulfamethoxazole | ≤ 0.5/95 | ≤ 2/38 | ---- | ≥ 4/76 | 3/0 |
| Vancomycinn | 1 | ≤ 2 | 4-8 | ≥ 16 | 4 |
Based on this information, daptomycin has the largest potential number of dilutions to resistance with vancomycin in second place. Since the organism appears resistant to sulfamethoxazole, that one is out. Daptomycin is much more expensive than the other medications, and is often held for approval by infectious disease, so let’s leave that one out. With vancomycin having twice as many dilutions as gentamicin, vancomycin would be the best drug.
In order to make this type of analysis and drug choice possible, our labs would have to report all of this information. Otherwise, this method isn’t practical. It would actually be better if our hospitals simply reported the number of dilutions needed to reach resistance rather than the MIC numbers. We would then have a logical approach to choosing antibiotics that would be better than simply going with what we are familiar with. As it stands, the current reporting methods open us up to an unfortunately missed opportunity. Hopefully this will change in the future.
Best wishes.

Jarrod Shapiro, DPM
PRESENT Practice Perfect Editor
[email protected]

























Comments
There are 0 comments for this article