
Paths to Practice Perfection
The Use of the 3M™ Dermatac™ Drape with NPWT: A Case Study Review
The Use of the 3M™ Dermatac™ Drape with NPWT: A Case Study Review
Patient
A 48-year-old female presented to the wound care center with a diabetic foot ulceration (DFU) that was present for three weeks. The patient had a great toe amputation as well as a partial amputation of the second toe from a previous diabetic foot infection. Initial symptoms on presentation included chills, erythema of her right foot, swelling, odor, and drainage (Figure 1). The DFU was probed to bone. The patient was admitted to the hospital for intravenous antibiotics. The patient had a WBC count of 18.1 and deep cultures were positive for moderate growth of Methicillin Resistant Staphylococcus aureus and moderate growth of Pseudomonas aeruginosa. Magnetic resonance imaging (MRI) suggested osteomyelitis of the remaining proximal phalangeal base and second metatarsal head. A multidisciplinary team approach for the patient care included specialists from podiatry, vascular surgery, internal medicine, infectious diseases, and wound care.
Co-morbidities
In addition to her diabetes, past medical history included diabetic peripheral neuropathy, obesity, fatty liver disease, gastroesophageal reflux disease, depression, and chronic nicotine use.
Course of Treatment
The patient was taken to the operating room for a 2nd ray amputation. The wound was left open due to the extent of infection (Figure 2). While in the acute hospital setting the patient’s diabetes and other medical conditions were managed by the hospitalist. Infectious diseases provided culture driven antibiotic therapy. On post-op day one packing from the open 2nd ray amputation was removed and traditional negative pressure wound therapy (NPWT) was started with a 3M™ V.A.C.® Ulta Therapy Unit at 125 mmHg continuous negative pressure. While in the hospital the patient was treated with the traditional acrylic drape with the 3M™ V.A.C.® Ulta Therapy Unit.

The patient was discharged on oral antibiotics, offloading, and a 3M™ ActiV.A.C.™ Therapy System to continue NPWT. On her first post-operative visit the patient’s surgical wound was macerated and NPWT was stopped for a week (Figure 3). The patient also had a 2.8 cm tunnel at the proximal dorsal wound (Figure 4). While the patient’s NPWT was stopped she was treated with 3M™ Promogran Prisma™ Collagen Matrix with ORC and Silver.
3M™ Promogran Prisma™ Collagen Matrix with ORC and Silver
3M™ Promogran Prisma™ Collagen Matrix with ORC and Silver modifies the chronic wound environment, inactivating potentially harmful proteases, oxygen free radicals and excess metal ions, while simultaneously protecting positive factors such as growth factors.1*
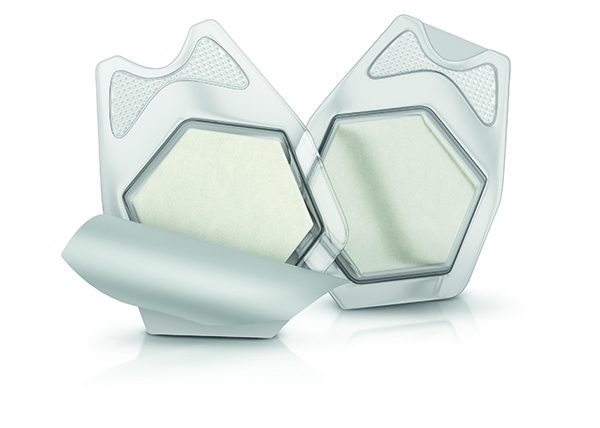
NPWT was resumed one week later and the traditional V.A.C.® acrylic drape was discontinued and replaced with the 3M™ Dermatac™ Drape, a silicone-acrylic hybrid drape.
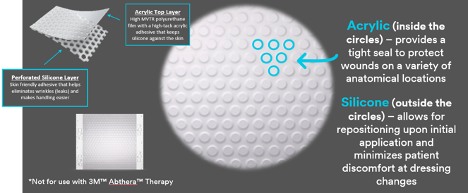
This demonstrates the unique construction of the Dermatac Drape.
What jobs should NPWT drapes do?
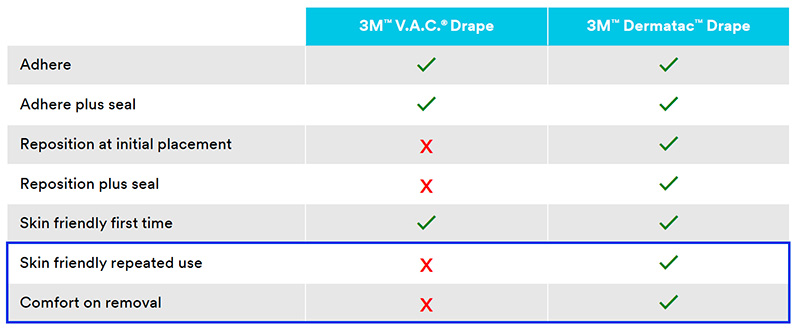
This shows us the differences between the standard V.A.C.® Drape and Dermatac Drape.
Through innovative dual technology, 3M™ Dermatac™ Drape works hard during each step of 3M™ V.A.C.® Therapy for clinicians and patients

Subjectively, the patient indicated increased comfort using Dermatac Drape, with less skin irritation and less pain during 3M™ V.A.C.® Dressing changes. The home health nurse shared ease of use with Dermatac Drape, reducing time spent during V.A.C.® Dressing changes.
The patient’s course was uneventful. The patient’s wound depth had significantly decreased with granulation tissue formation close to the peri-wound skin after 20 days using the ActiV.A.C. Therapy System along with Dermatac Drape at 125 mmHg continuous negative pressure (Figure 5). The ActiV.A.C. Therapy System and Dermatac Drape were discontinued, and the patient’s wound care was changed to Promogran Prisma Matrix three times per week. The patient’s surgical wound went on to full closure at post-operative day 78 (Figure 6). Offloading was maintained throughout the post-operative course. The patient was referred to Prosthetics and Orthotics and received extra-depth diabetic shoes and custom insoles.
Treatment Modalities
- Multidisciplinary team approach
- Open 2nd ray amputation
- IV Vancomycin
- IV Cefepime
- Oral Flagyl
- 3M™ V.A.C.® Ulta Therapy Unit
- 3M™ ActiV.A.C.™ Therapy System
- 3M™ Dermatac™ Drape
- 3M™ Promogran Prisma™ Collagen Matrix with ORC and Silver

(Figure 1) Infected diabetic foot ulceration

(Figure 2) Open 2nd ray amputation

(Figure 3) Macerated wound, NPWT discontinued for a week

(Figure 4) Wound with 2.8 cm tunnel

(Figure 5) Wound with granulation tissue, wound care changed to 3M™ Promogran Prisma™ Collagen Matrix with ORC and Silver

(Figure 6) Full closure on post-operative day 78
Conclusion
This case study reviewed the treatment plan for an infected DFU with osteomyelitis that included an open 2nd ray amputation, NPWT, and the new silicone acrylic Dermatac Drape. The wound was then managed with Promogran Prisma Matrix and went on to closure.
Do you have questions regarding this case study?
Request a sample or connect with a 3M Account Representative
As with any case study, the results and outcomes should not be interpreted as a guarantee or warranty of similar results. Individual results may vary depending on the patient’s circumstances and condition.
NOTE: Specific indications, contraindications, warnings, precautions, and safety information exist for these products and therapies. Please consult a clinician and production instructions for use prior to application. Rx only.
© 2022 3M. All rights reserved. 3M and the other marks shown are marks and/or registered marks. Unauthorized use prohibited.
*in-vitro
References
- Gottrup F, Cullen B, Karlsmark T, Bischoff-Mikkelsen M, Nisbet L, Gibson M. Randomized controlled trial on collagen/oxidized regenerated cellulose /silver treatment. Wound Repair & Regeneration. 2013;21:1-10.

Comments
There are 0 comments for this article